Welcome to your best chiropractic year!
Commercial health insurance carriers such as United Health Care and Anthem BCBS can offer their customers, who are also your patients’ employers, two different health account savings options:
- Health Reimbursement Arrangement
- Health Savings Account
An employer can also directly offer the benefit of their employees signing up for a Flexible Spending Account.
Let’s dig into each one!
What is a Health Reimbursement Account? (HRA)
A Health Reimbursement Account (HRA) is an account that your patient’s employer funds to help the employee pay for covered healthcare services. The patient cannot put monies into an HRA, as the account is owned by the employer. This includes paying for services (chiropractic office visits) that apply to the patient’s deductible. The patient can begin using their HRA on the first day of the plan year. Since the patient’s employer controls the fund, the employer has the ability to make the rules on when and how the patient can use the money. Additionally, there are coinsurance-only HRA plans available, whereby the patient’s employer will pay only coinsurance amounts.
The patient does not have to pay taxes, state or federal, on HRA monies, so it is a tax savings. The HRA cannot earn interest as it is not a personal bank account.
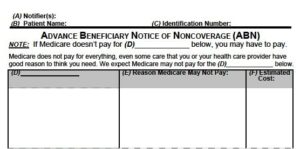
How do you, Doctor, get paid? Once claims are submitted to the insurer, the insurance carrier will pay, as long as the patient has funds in the account. You will typically, but not always, receive two EOBs/remittances for the same DOS. This is usually due to that first charge going to the patient’s PCP and then getting denied and forwarded to the employer. Referrals from the patient’s PCP to your office is not a requirement tied to an HRA.
There is only one account set up for all covered dependents on a plan. The employee does not report the HRA monies to the IRS.
Takeaways:
- Get in good standing with your community’s businesses and industries so chiropractic can stay included on their coverage and benefits, and you can get those referrals!
- Billing Tip: Make sure you are posting to the most recent, newest remittance.
Health Savings Account (HSA)
A Health Savings Account is a savings plan set aside for taxpayers who enroll themselves in a high-deductible health plan. They can be offered by your patient’s employer as an employee benefit, or the patient may elect to sign up independently. The benefit here is that the funds are not subject to tax liability upon deposits. Moreover, if there are monies left in an HSA, they can roll over into the next year. When your patient’s health plan offers this type of plan, they are provided with a debit or credit card to make their eligible health service purchases. Both the patient and their employer can contribute to the fund. The patient must report this account to the IRS when they do their taxes.
Takeaway:
Health Savings Accounts are not owned by the patient’s employer. All taxpayers with high-deductible health plans are eligible and must report this account to the IRS when doing taxes.
Employer-based Flexible Spending Accounts (FSA)
An Flexible Spending Account is a special account the patient puts money into to pay for certain out-of-pocket expenses such as medical related, dependency related, and a limited dental and vision plan. This arrangement also has a tax-free benefit. The list of all eligible expenses can be found on the IRS website at: https://www.irs.gov/newsroom/irs-plan-now-to-use-health-flexible-spending-arrangements-in-2019
The employer owns this account.
A frequently asked question I get is, does an FSA cover massage?
Answer: Yes, it does with the ordering physician (chiropractors included) writing a note of necessity for the massage therapy.
When there are monies left over in the account at the end of the year, the employer has two options they can offer their employees:
- The patient can set aside the monies and use it up to two-and-a-half months into the new year, or
- The employer can allow the employee to carry over up to $500 from one year to the next.
Takeaway:
There are several eligible out of pocket expenses that an FSA will cover. Click on the IRS link for more information: https://www.irs.gov/newsroom/irs-plan-now-to-use-health-flexible-spending-arrangements-in-2019
SUMMARY
If your patients struggle to keep their appointments due to financial concerns ask them if they have one of these savings accounts that might be able to supplement payment of their care and keep them on their treatment plan.
Oh, one further heads-up to our profession just finding its way down the pipeline . . . you may have or will be receiving a letter from a TriWest Family Alliance group out of Arizona promoting their billing services on behalf of VA offices. This letter is being distributed nationwide. Please note we have researched this, and credentialing and contracting with this group is optional. If you already have a contract with your VA, you may continue treating VA patients as usual. There is no change in their referral of patients to you, or the preauthorization process.
If you have any further questions, don’t hesitate to reach out to either myself or Dave.
Please feel free to forward this article to your insurance department.
Adios for now!
Lisa
“Increasing your collections through better billing and documentation.”